Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
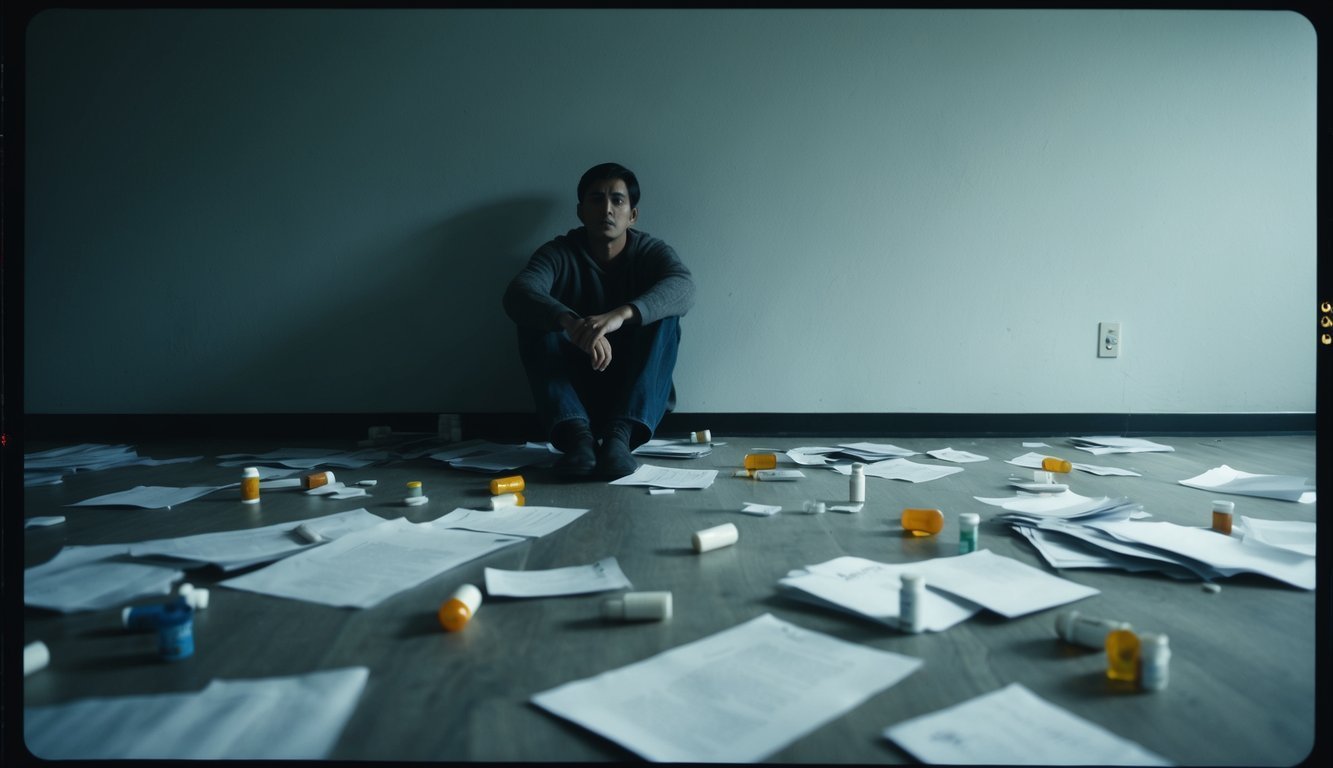
Major Depressive Disorder significantly impacts mood, cognition, and behavior, characterized by persistent sadness, loss of interest, and functional impairments, affecting millions globally.

Major Depressive Disorder (MDD) is a multifaceted mental health condition that profoundly influences mood, cognition, and behavior.
This disorder is marked by enduring feelings of sadness, a loss of interest in activities, and disruptions in daily functioning.
Major Depressive Disorder is categorized as a mood disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
It belongs to the broader class of depressive disorders, which includes conditions such as Persistent Depressive Disorder and Premenstrual Dysphoric Disorder.
The diagnosis of MDD requires the presence of specific symptoms that have persisted for at least two weeks.
These symptoms must denote a noticeable alteration from previous functioning and result in significant distress or impairment in social, occupational, or other important areas of functioning.
The DSM-5 outlines clear diagnostic criteria for MDD, assisting healthcare professionals in distinguishing it from other mood disorders and ensuring accurate assessments.
The core symptoms of MDD consist of:
A diagnosis requires at least five of these symptoms, with either a depressed mood or loss of interest being one of them.
The intensity and duration of symptoms can differ significantly among individuals.
Depression is a prevalent mental health condition affecting millions globally.
The prevalence of MDD differs across various demographics and regions.
Research shows that women are more frequently affected by MDD than men.
The disorder can manifest at any age, though it typically emerges in the mid-20s.
Lifetime prevalence rates for MDD range from 10% to 20% in many countries.
Factors influencing these rates include genetic predisposition, life stressors, and socioeconomic status.
MDD often occurs alongside other mental health disorders, such as anxiety disorders or substance abuse disorders, complicating both diagnosis and treatment.

Major Depressive Disorder is influenced by intricate interactions between neurobiological mechanisms and psychological factors.
These elements significantly impact the emergence, course, and management of depression.
The brain’s chemistry is vital in understanding depression.
Those with Major Depressive Disorder often have dysregulated neurotransmitters such as serotonin, norepinephrine, and dopamine, with serotonin deficiency being particularly linked to depressed mood and anxiety.
Brain imaging studies have identified both structural and functional alterations in individuals suffering from depression.
For instance, the hippocampus, which plays a role in memory and emotion regulation, may show atrophy, and the amygdala, involved in emotion processing, may demonstrate increased activity.
Furthermore, glutamate, an excitatory neurotransmitter, is receiving attention in depression research, as atypical glutamate signaling may play a role in mood disruption and cognitive difficulties.
Psychological elements greatly shape the development of depression.
Early-life trauma can heighten one’s susceptibility to depressive episodes later on.
Additionally, chronic stress can activate the body’s stress response system, potentially leading to long-term modifications in brain function.
A family history of depression often contributes to risk, intertwining genetic make-up with environmental influences.
Those with relatives who have experienced depression are at an elevated risk.
Cognitive styles characterized by negative self-image and pessimism can also exacerbate depressive symptoms. Cognitive Behavioral Therapy addresses these cognitive patterns, assisting patients in developing more constructive thought strategies.
Comorbidity with anxiety is frequent, complicating the clinical picture, as each condition can potentially worsen the other.

The diagnosis of major depressive disorder necessitates a thorough evaluation utilizing standardized criteria and assessment tools.
Clinicians must meticulously analyze symptoms to differentiate MDD from other mental health issues.
The Diagnostic and Statistical Manual of Mental Disorders (DSM) serves as the principal reference for diagnosing major depressive disorder.
Healthcare providers utilize these guidelines to evaluate the presence, duration, and intensity of depressive symptoms.
Key diagnostic elements involve:
The Patient Health Questionnaire-9 (PHQ-9) is a widely recognized screening instrument aligned with DSM criteria, facilitating the quantification of symptom severity and tracking changes over time.
Mental Status Examinations offer additional insights into a patient’s cognitive function, appearance, and behavior, supplementing self-reported symptoms to paint a full diagnostic picture.
Identifying major depressive disorder amidst other mental health issues is vital for delivering appropriate treatment.
Clinicians must consider various potential alternatives during the diagnosis.
Anxiety disorders commonly accompany depression and can present overlapping symptoms, necessitating careful examination of the primary indicators and their onset timelines for accurate diagnosis.
Bipolar disorder may exhibit characteristics similar to major depressive disorder during low mood episodes.
Clinicians must investigate any history of manic or hypomanic episodes to differentiate between the two.
Substance abuse disorders can also induce depressive symptoms, making comprehensive substance use histories and periods of abstinence key factors in diagnosis.
Psychotic disorders, such as schizophrenia, can encompass depressive aspects.
Evaluating the presence of hallucinations, delusions, or disorganized thought processes is integral to differentiate these conditions accurately.
Medical issues such as thyroid dysfunctions or neurological disorders can mimic depressive symptoms, necessitating comprehensive medical evaluations to rule out these potential contributors.
Effective treatment for major depressive disorder comprises a blend of pharmacological therapies, psychotherapeutic techniques, and innovative treatment options aimed at alleviating symptoms, enhancing life quality, and preventing relapse.
Antidepressant medications form the foundation of pharmacological treatment for major depressive disorder.
Selective Serotonin Reuptake Inhibitors (SSRIs) are often the first choice given their effectiveness and manageable side effect profiles.
Common SSRIs include fluoxetine, sertraline, and escitalopram.
Although less frequently prescribed, tricyclic antidepressants still prove effective for certain patients by increasing norepinephrine and serotonin levels.
Examples include amitriptyline and nortriptyline.
Atypical antidepressants, such as bupropion and mirtazapine, offer alternative mechanisms of action and can be particularly advantageous for individuals who do not respond positively to SSRIs or experience unwanted side effects.
Table: Common Antidepressant Classes
| Class | Examples | Primary Mechanism |
|---|---|---|
| SSRIs | Fluoxetine, Sertraline | Boost serotonin levels |
| Tricyclics | Amitriptyline, Nortriptyline | Enhance serotonin and norepinephrine levels |
| Atypicals | Bupropion, Mirtazapine | Diverse mechanisms |
Cognitive Behavioral Therapy (CBT) stands out as an effective psychotherapeutic approach for treating major depressive disorder.
It assists patients in identifying and altering negative thoughts and behaviors contributing to depressive symptoms.
Interpersonal therapy works to enhance relationships and communication skills, providing significant benefits particularly for individuals whose depression is related to social interactions or relationship issues.
Psychodynamic therapy delves into unconscious conflicts and past experiences that may influence current depressive symptoms, fostering insight and facilitating long-term personal development.
Group therapy provides a supportive space for individuals to share experiences and learn from peers facing similar challenges, offering an affordable option with valuable social support.
Electroconvulsive Therapy (ECT) continues to be a viable option for severe or treatment-resistant depression, with modern techniques improving safety and minimizing side effects compared to past practices.
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate targeted areas of the brain.
It has shown potential for treating depression, particularly in patients who do not respond to traditional medications.
Ketamine therapy has emerged as a novel treatment for treatment-resistant depression, providing rapid symptom relief when administered in controlled environments.
Digital mental health tools, including smartphone applications and online therapy platforms, are broadening access to treatment methods.
These resources can augment conventional therapies and provide support between sessions.

Major Depressive Disorder (MDD) can have severe repercussions on an individual’s life and overall health.
It often leads to substantial impairments in daily functioning and heightens the risk of other health conditions.
MDD can significantly undermine an individual’s quality of life.
People may endure relentless sadness, hopelessness, and an inability to find pleasure in previously enjoyable activities.
Common sleep issues may occur, with some individuals facing excessive sleep while others confront insomnia, leading to fatigue and diminished energy levels that negatively affect work and social life.
Cognitive dysfunction is another critical outcome.
MDD can impair concentration, memory, and decision-making skills, potentially obstructing academic or professional achievements.
In extreme cases, MDD can lead to suicidal thoughts or actions, prompting the need for immediate mental health interventions.
MDD frequently coexists with other mental health disorders, complicating diagnosis and therapeutic strategy.
Anxiety disorders are often seen alongside depression, intensifying symptoms and reducing overall functionality.
Individuals with MDD may also experience substance use disorders, as some turn to alcohol or drugs for self-medication, creating a problematic cycle of addiction and worsening depression.
Certain forms of depression related to hormonal changes are more prevalent in women, including premenstrual dysphoric disorder, postpartum depression, and perinatal depression.
Adjustment disorders and panic disorder may also manifest alongside MDD, further hindering an individual’s ability to cope with daily stresses and maintain healthy relationships.
“`